Acupuncture has been clinically refined for over 4000 years and has the most extensive clinical case study history of any medical practice, yet there still remains gaps in research, education and understanding in the mainstream western medical paradigm.
How Effective is Acupuncture for Pain Relief
However, evidence for the effects of acupuncture on pain are substantive. In a study that consolidated outcome measures for pain and function from 39 trials and 20,827 patients found that acupuncture had superior results to sham acupuncture and the no acupuncture control group and, remarkably, the effects of acupuncture persists over time with only a small decrease (~ 15%) in treatment effect at 1 year. The study concluded that acupuncture is particularly effective for chronic pain. Another study demonstrated that acupuncture is particularly effective for treatment of migraines and fibromyalgia, which are two of the most complex pain conditions to treat.
Even without the proof from this analysis of evidence-based research, acupuncture has survived and flourished because it works so well. But there is still confusion from Western medical professionals and patients alike – how does it work from a biomedical perspective?
Biomedical Insights into Acupuncture
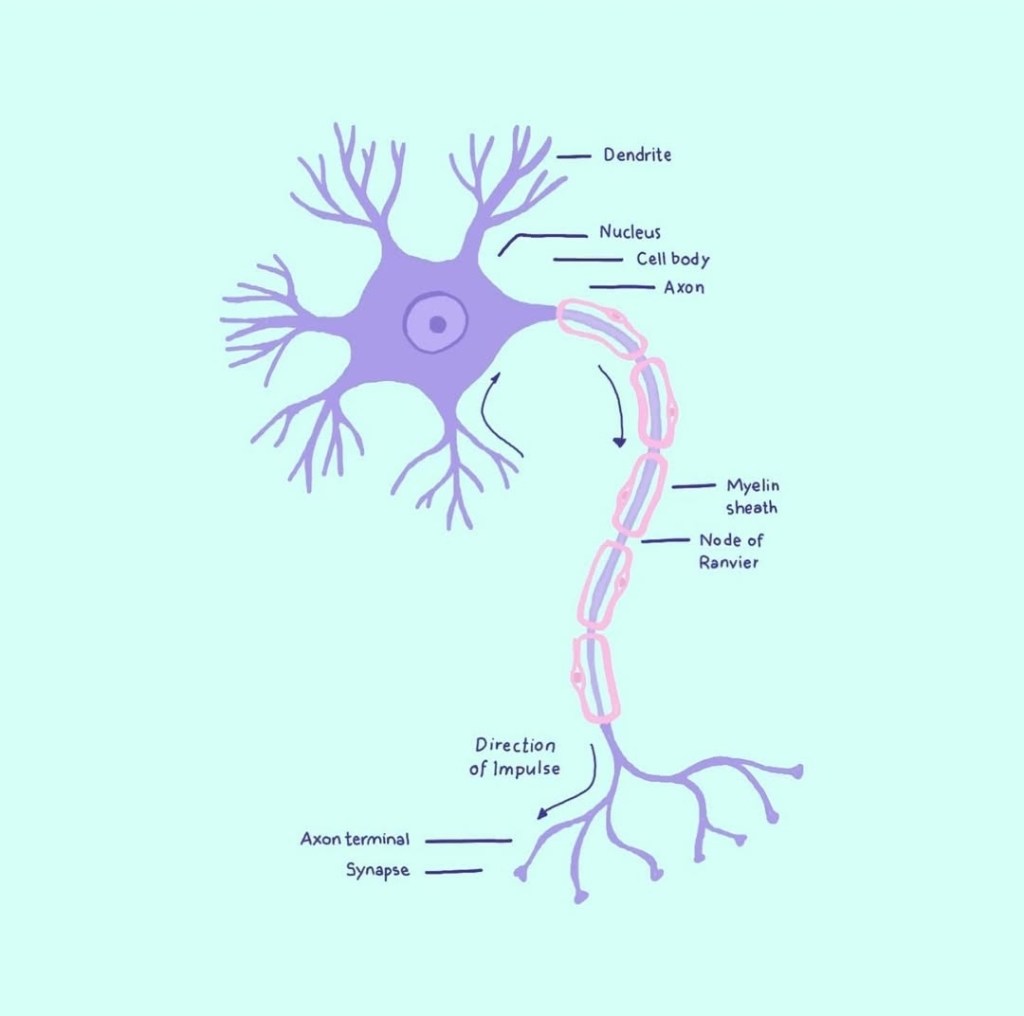
Studies on electroacupuncture mechanisms reveal that electroacupuncture activates the nervous system differently for pain conditions than in healthy subjects, alleviates both sensory and affective inflammatory pain, and inhibits inflammatory and neuropathic pain. Electroacupuncture blocks pain by activating a variety of bioactive chemicals through peripheral, spinal and supraspinal mechanisms, including opioids, serotonin and norepinephrine. Additional studies suggest that electroacupuncture, when combined with low dosages of conventional analgesics, provides effective pain management which can forestall the side effects of often debilitating pharmaceuticals.
In simpler terms, acupuncture triggers our nervous system to release tension, and switch from a sympathetic (fight and flight) state to a parasympathetic (rest and digest) state. It is in the parasympathetic state that the body is able to heal itself and allows the body to reset, detoxify, and regenerate. Locally, acupuncture releases endogenous opioids to relieve pain.
Neuroscience and Fascia
In a study on the effects of acupuncture on depression, the study found that acupuncture could modulate the brain in several ways. The study conducted MRI brain scans while different acupuncture points were needled, which revealed activity in various areas of the brain depending on the point stimulated. This proposes that there is a neuroscientific component to acupuncture efficacy, an area of study that is gaining traction in acupuncture research in the US.
So what is a channel? Channel or meridian theory is a foundational aspect of Traditional Chinese Medicine and directs how and why we place and manipulate acupuncture needles for therapeutic effect. Studies have found evidence that the fascia may be the physical substrate for acupuncture channels. Fascia connective tissue contains nerve endings, capillary vessels, fibroblasts, undifferentiated mesenchymal cells, lymphocytes and so forth. The distribution of fascia connective tissue throughout the body and enables acupoints to exist in every part of the body and produces both local and systemic reactions when stimulated in specific ways.
Clearly, acupuncture is complex and works on many levels simultaneously. Acupuncture stimulates the peripheral nervous system, the brain, the vascular system, the fascial network, promotes circulation and oxygenation, releases bioactive chemicals, regulates inflammatory markers and beyond. In the words of Dr. Sonia Tan, acupuncturists are neurovascular microsurgeons.
References:
Bai Y, Wang J, Wu JP, Dai JX, Sha O, Tai Wai Yew D, Yuan L, Liang QN. Review of evidence suggesting that the fascia network could be the anatomical basis for acupoints and meridians in the human body. Evid Based Complement Alternat Med. 2011;2011:260510. doi: 10.1155/2011/260510. Epub 2011 Apr 26. PMID: 21584283; PMCID: PMC3092510.
https://pmc.ncbi.nlm.nih.gov/articles/PMC3092510/
Zhang J, Wu X, Nie D, Zhuo Y, Li J, Hu Q, Xu J, Yu H. Magnetic Resonance Imaging Studies on Acupuncture Therapy in Depression: A Systematic Review. Front Psychiatry. 2021 Aug 20;12:670739. doi: 10.3389/fpsyt.2021.670739. PMID: 34489749; PMCID: PMC8417590.
https://pmc.ncbi.nlm.nih.gov/articles/PMC8417590/
Vickers AJ, Vertosick EA, Lewith G, MacPherson H, Foster NE, Sherman KJ, Irnich D, Witt CM, Linde K; Acupuncture Trialists’ Collaboration. Acupuncture for Chronic Pain: Update of an Individual Patient Data Meta-Analysis. J Pain. 2018 May;19(5):455-474. doi: 10.1016/j.jpain.2017.11.005. Epub 2017 Dec 2. PMID: 29198932; PMCID: PMC5927830.
https://pubmed.ncbi.nlm.nih.gov/29198932/
Zhang R, Lao L, Ren K, Berman BM. Mechanisms of acupuncture-electroacupuncture on persistent pain. Anesthesiology. 2014 Feb;120(2):482-503. doi: 10.1097/ALN.0000000000000101. PMID: 24322588; PMCID: PMC3947586.
https://pubmed.ncbi.nlm.nih.gov/24322588/
Patel M, Urits I, Kaye AD, Viswanath O. The role of acupuncture in the treatment of chronic pain. Best Pract Res Clin Anaesthesiol. 2020 Sep;34(3):603-616. doi: 10.1016/j.bpa.2020.08.005. Epub 2020 Aug 8. PMID: 33004170.

Leave a comment